COLORECTAL CONUNDRUMS
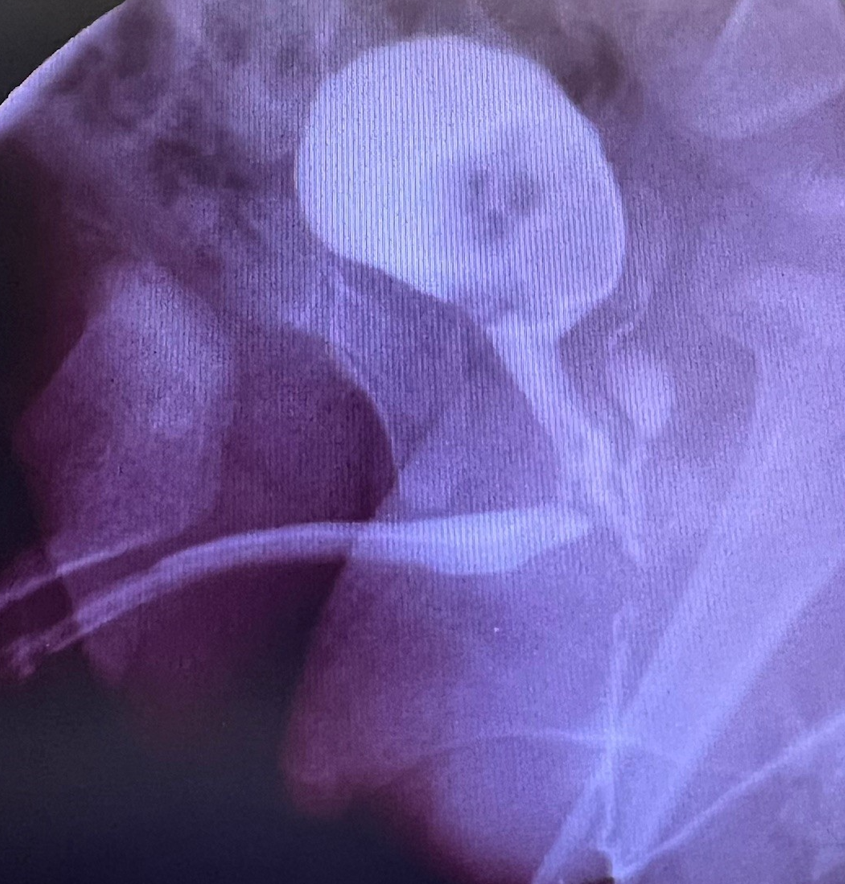
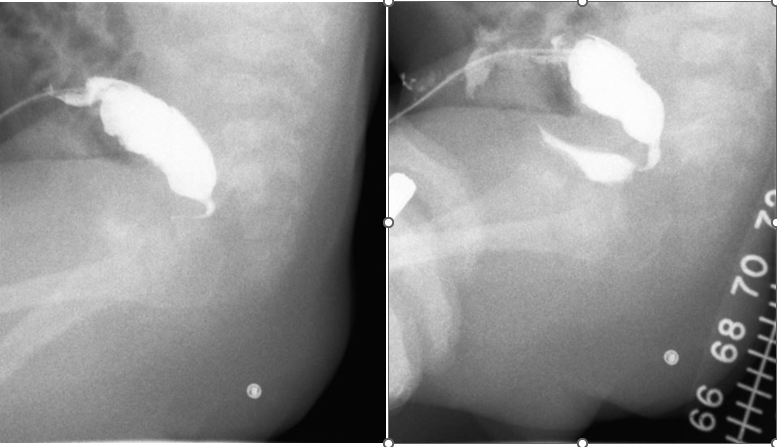
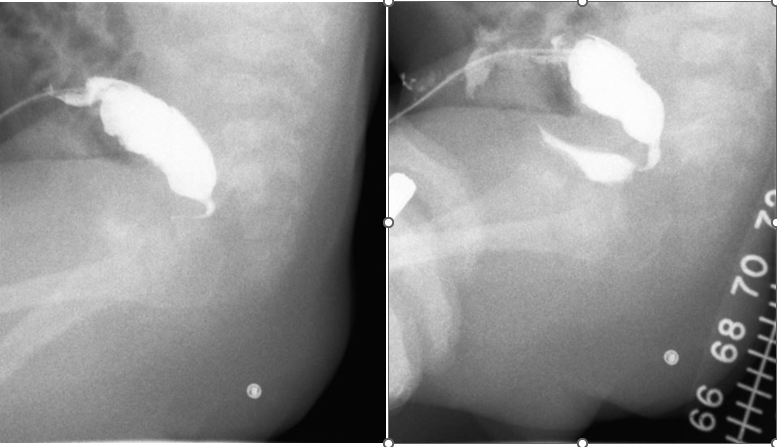
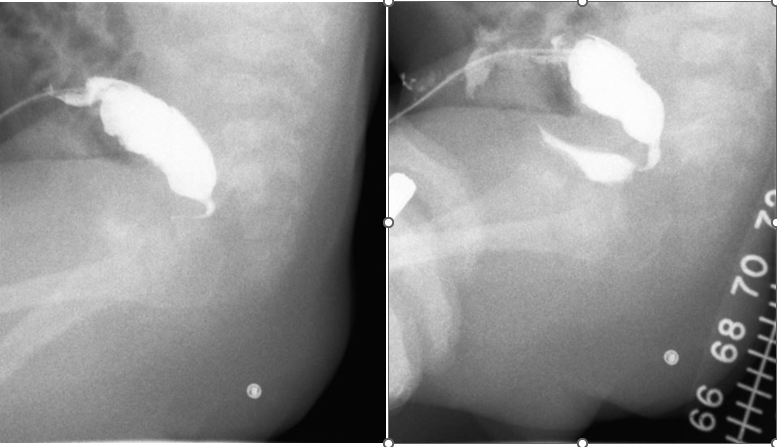
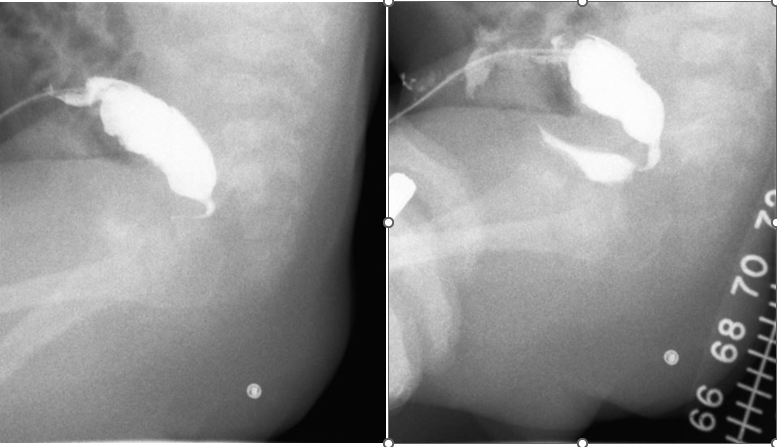
Colorectal Conundrum for January 29: A male with a rectoperineal fistula undergoes a PSARP with mobilization of the rectum, both anterior and posterior rectal walls. In the days following surgery he starts to drain urine around the anoplasty consistent with a urethral injury. He is also voiding via the penis. A cystogram is shown below. How would you manage this situation? Answer: This patient has suffered from a urethral injury, and urine is draining out the posterior urethra into the perineum around the anoplasty. The key first step is to divert the urine with a suprapubic tube. A colostomy is not necessarily needed. The fistula might heal with diversion. If after a month or so a cystogram shows the persistence of the fistula, then a redo is needed with re-mobilization of the rectum, fully lifting the anterior rectal wall off of the urinary tract, and repair the urethra, with coverage of the posterior urethra with an ischiorectal fat pad. Then a voiding trial a month later with ultimate removal of the SP tube.
Colorectal Conundrum for January 22nd: In the previous week’s case, of an imperforate hymen, the MRI showed dilation all the way down to the perineum. Management involved a perineal – introital – incision to drain the fluid. If that were not the case and you had a dilated vagina but the distal extent was far away from the introital area, how might you handle that hydrocolpos? Answer: If this were a case of hydrolpos with normal anus and normal urethra, and the vagina cannot be drained by the introitus like an imperforate hymen, then drainage needs to be from above. IR or laparoscopy is an ideal approach to get a drain in the dilated structure (remember this could be bilateral, so both sides may need to be drained. Drainage is to relieve distension and most concerning its potential cause of distal ureteral obstruction causing hydronephrosis. Once the material hormones have dissipated the hydrocolpos will resolve and can be dealt with later in life via a laparoscopic distal vaginal pull-through, after the onset of puberty. In such a patient, I would follow closely with ultrasound 6 months after thelarche (breast budding).
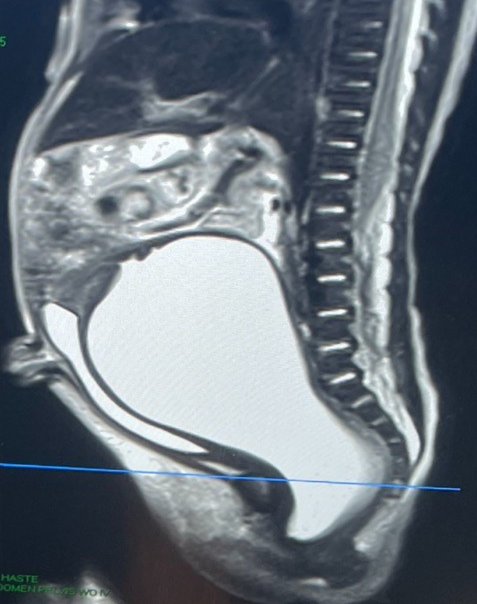
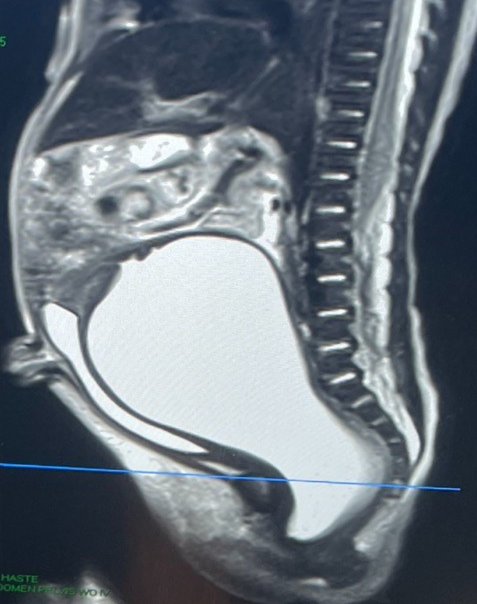
Colorectal Conundrum for January 16: A newborn female is noted to have abdominal distension. On exam the uretha and anus are normal, and there appears to be a bulge in the hymen. The has an MRI with the image shown below. What would be your treatment plan? What are the variations in such a case and how would you manage each? Answer: This could be a case of imperforate hymen, but the MRI is key – how high up is the obstruction? How large is the hydrocolpos? In this case, it appears that a perineal incision might all that is needed as the dilation extends all the way down to the perineum. That is the most common scenario. An incision at the level of the hymen should drain out the fluid and no further intervention should be needed. Of course a careful exam needs to check to be certain you see a urethra – sometimes such a bulge could be a paraurethral cyst. For the next week’s question – what would you do if the perineal approach was inadequate – i.e. could not reach the dilated lumen.

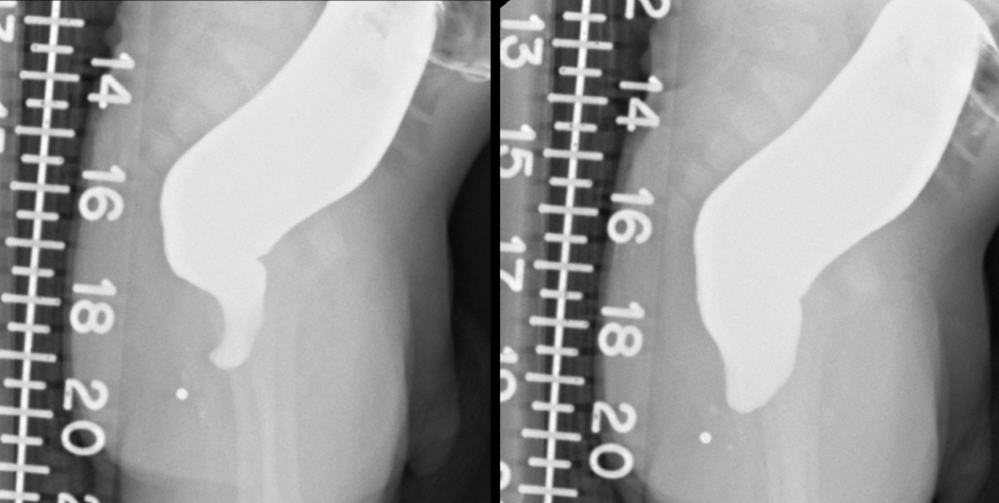
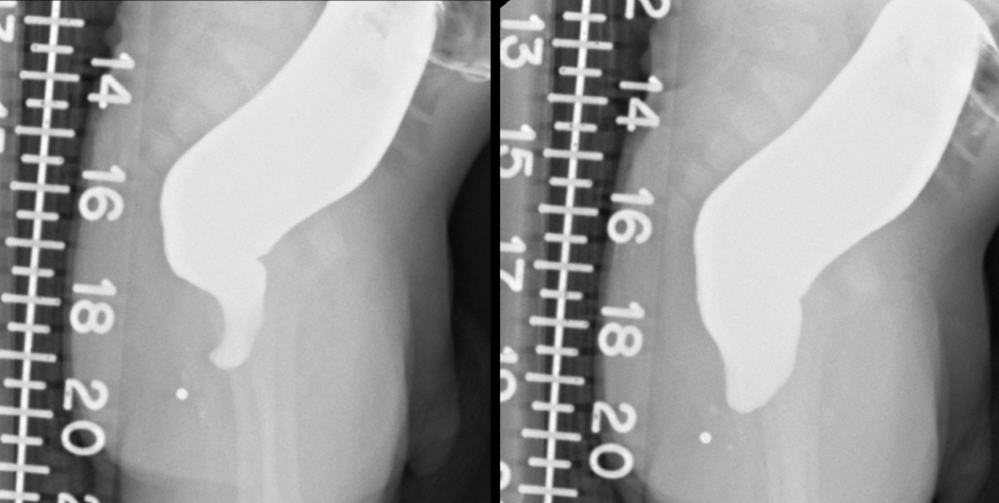
Colorectal Conundrum for January 8: A newborn is diagnosed with HD by suction rectal biopsy and this is the contrast study. The biopsy shows no ganglion cells and hypertrophic nerves, but the pathologist notes significant inflammation. Irrigations are going well, and the abdomen is soft and flat. What would you do? Proceed with pull-through or send home on irrigations and delay the pull-through for several months. Which is your usual routine? Does the pathology findings influence that decision? Answer: This is a relatively common conundrum for the surgeon, taking care of patient with diagnosed HD, doing well on irrigations, but recovering from HAEC, or on biopsy showing evidence of inflammation. In such a case I would be inclined to do longer term irrigations, send the baby home (provided irrigations are going well), and do the pull-through for what looks like typical sigmoid disease at 2 to 3 months of life.
Colorectal Conundrum for December 18th: The prior Conundrum case of rectal atresia warrants more discussion. Both of the surgery to solve the problem and what to do about the presacral mass if one is found. Let’s start with the mass. If a presacral mass is identified on imaging and there is no dural components what would you do? If there is a dural connection, what would you do in that case? Answer: If a presacral mass is identified (on pelvic MRI) and there is no spinal component (on spinal MRI) then the mass can be removed at the time of the anal repair (see prior response for the operative approach). If there is a dural connection then the mass should be removed via a posterior sagittal approach first (in collaboration with neurosurgery) and the anal work delayed for a future date.
Colorectal Conundrum for December 11th: Newborn with normal appearing anus but distended and anal probe didn’t go in more than 1 cm. Surgeons performed an anal exploration, didn’t find a lumen, and then decided to do a colostomy. Below is the distal colostogram. Questions: How do you explain the funny looking presacral space? What is the likely diagnosis here? What work-up is vital to rule out a key associated problem?
For the Quiz & Answers to last weeks Conundrum - see the blog post here . Colorectal Conundrum for December 4th: A 9-year-old female with Hirschsprung disease underwent a Yancey-Soave pull-through in the first year of life. She developed constipation and for this was treated with a myectomy. She began to have soiling and also was noted to pass stool via the vagina and for this was diverted with an ileostomy. On your exam her dentate line is absent and her sphincters are patulous, confirmed by anorectal manometry as weak particularly on the left side. She has a rectovaginal fistula and a palpable circumferential cuff. What would you offer this patient. Answer: This patient is diverted with an ileostomy, and we need to explain why they needed this diversion – i.e. Is there a distal obstruction? What do we do about the rectovaginal fistula? She has a missing dentate line and patulous sphincters. And a palpable cuff. She needs a redo – repair of the rectovaginal fistula, removal of the cuff, and confirmation that there are good ganglion cells present at the distal pull-through. As for the patulous sphincters – the pull-through can be tacked to the perineal area musculature to perform a sphincter reconstruction. Here is a useful video of a similar case: https://www.expertsinsurgery.com/programs/sphincter_reconstruction_withlogo-3192d1?category_id=49506
For the Quiz & Answers to last weeks Conundrum - see the blog post here . Colorectal Conundrum for November 27th: An 8-year-old female with Hirschsprung disease and Trisomy 21 had a colostomy and then a colostomy pull-through with appendectomy, but due to stricture required a redo of the pull-through. She has no evidence on exam of a dentate line. The child has been doing well on rectal enemas. The child is now becoming resistant to the rectal enemas. What are the options and what would you recommend for this patient? Answer for November 27th: With a missing dentate line, potential for bowel control is questionable. She has done well on rectal enemas, but given that she is resistant to them now, an antegrade option could be considered. Either a neoMalone made with a flap of cecum or a cecostomy – my preference is a neoMalone which allows her to be cathed. Here is a nice video: https://www.expertsinsurgery.com/programs/malone-mitrofanoff-nchmp4-7b8609?category_id=49506
For the Quiz & Answers to last weeks Conundrum - see the blog post here . Colorectal Conundrum for November 20th: 5 year-old-boy with an ARM, poor sacrum and tethered cord, needed to undergo a redo of his PSARP for prolapse. He has bilateral vesicoureteral reflux, a strictured urethra, and poor bladder emptying – for this he has a vesicostomy. His reflux has recently worsened, and it is believed this is due to constipation, despite treatment with laxatives. From a urologic point of view he needs a Mitrofanoff and ureteral reimplanation but he is not ready for that - he won’t cath. What would you do to manage his constipation given how troubling this is to his urinary system? Answer: This patient would benefit from antegrade flushes, but also likely needs a Mitrofanoff in the future. One strategy we have employed in this situation is to do a nonplicated Malone. I bring the tip of the appendix to the RLQ skin using laparoscopy and simply suture it there, mucosa to skin, and place a tube. Then the patient can have antegrade flushes, and in the future this can be taken down and the appendix used for a Mitrofanoff either its full length, with creation of a neoMalone, or split into Malone and Mitrofanoff.
For the Quiz & Answers to last weeks Conundrum - see the blog post here . Colorectal Conundrum for November 13th: What would you do in this male patient with ARM, newborn colostomy, and now with distal colostogram showing the below finding? Answer for November 13th: There is much more to this case than meets the eye and several options. The key item to recognize is the very high rectum and short distal piece of bowel given the location of the colostomy. One choice would be to take down the fistula laparoscopically and pull it through, but I caution against leaving a Hartman’s pouch in – the colostomy closure will be super difficult. So one could close the colostomy and then divert above with a more proximal colostomy or with an ileostomy. However, given the potentially poor blood supply of this piece of rectum and to avoid two anastomoses (anoplasty and colo-colonic), plus the new diversion and the stoma closure that goes along with it, and seeing how poor is the sacrum, my choice here would be to pull through the colostomy and remove this distal piece. I know how important is the rectum to provide a reservoir and allow for continence but I am balancing all of that surgery with a likely incontinent child here that would do fine with a sigmoid pulled through and antegrade flushes via the Malone.