Colorectal Conundrum: October 9, 2023
For Quiz & Answers to the October 2nd Conundrum - see the blog post here.
Colorectal Conundrum for October 9th:
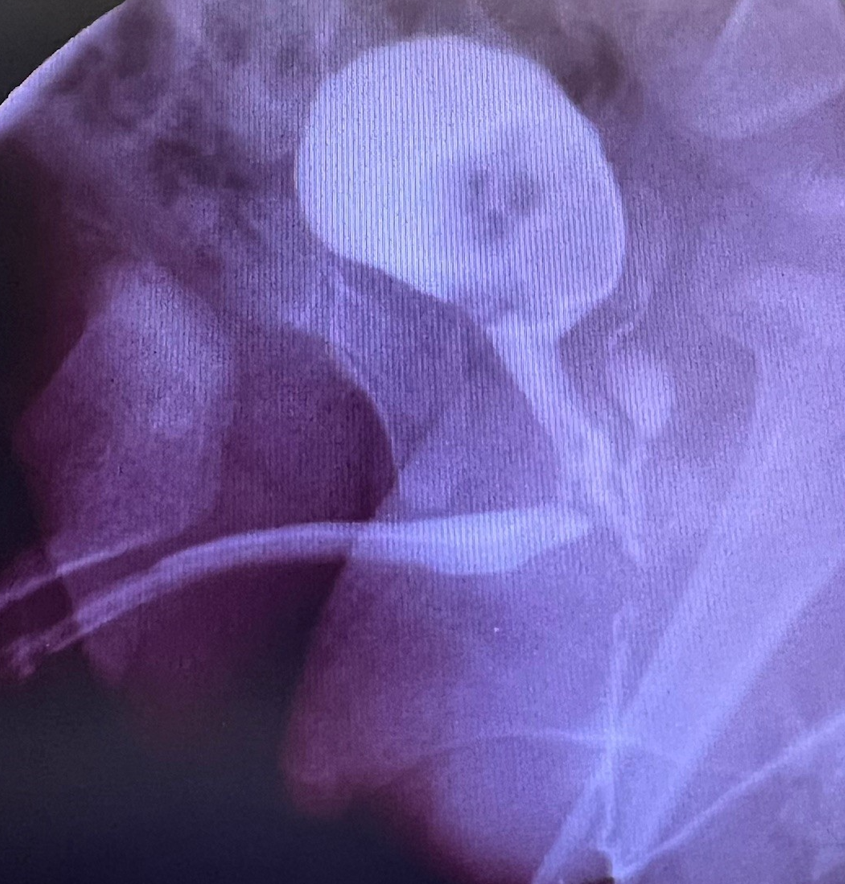
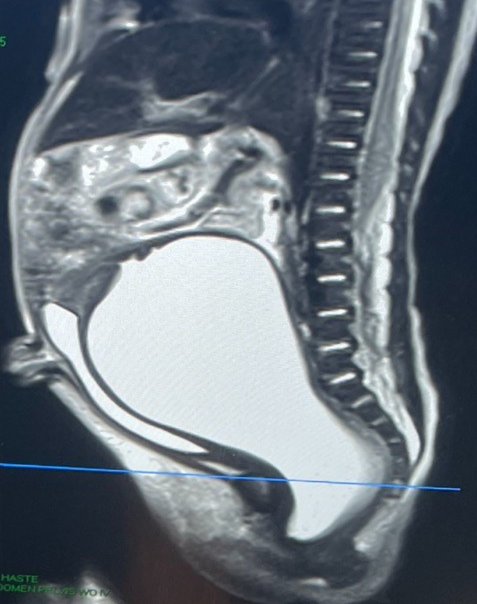
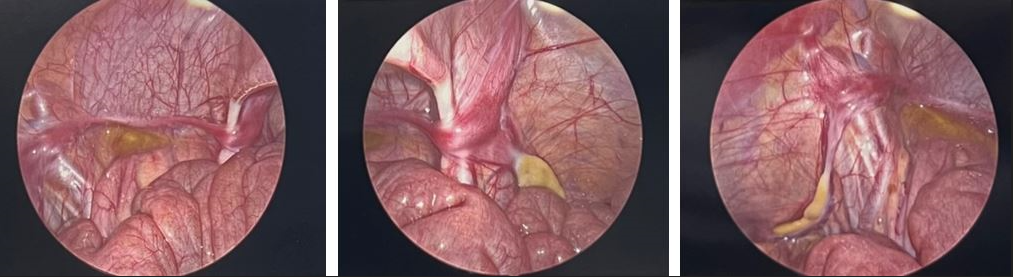
A patient with a cloaca undergoes cystoscopy and a urethra is identified and a rectal fistula but no orifice for a vagina is seen. The cloacagram is shown as is the view done by a diagnostic laparoscopy. What is your interpretation of this patient’s cloacal anatomy and of her intraabdominal Mullerian anatomy?
Answer for October 9th:
This rare cloaca has a common channel that goes directly into the bladder. There is only a rectal fistula and no distal vagina at all on scope. Laparoscopy shows Mullerian remnants. It is impossible to know at this point what will become of those structures upon hormonal stimulation at puberty. So the ideal treatment is to perform that rectoplasty via a PSARP approach and leave the common channel alone and disconnect the rectal fistula from the good lumen rectum and close it over with absorbable suture. At puberty, a pelvic ultrasound after thelarche would reveal if there is growth of the vagina, and if so, that structure could be pulled through the old rectal fistula removed. If no Mullerian structures develop the rectal fistula could be dilated at a later age when the patient is able to do that.

How would you handle this case?